Ketones in the urine, as detected by urine testing stix or a blood ketone testing meter[1], may indicate the beginning of diabetic ketoacidosis (DKA), a dangerous and often quickly fatal condition caused by low insulin levels combined with certain other systemic stresses. DKA can be fixed if caught quickly.
Emergency Info
Diabetics of all species therefore need to be checked for ketones whenever insulin level may be too low, and any of the following signs or triggers are present:
|
Ketone Monitoring Needed: | |
|---|---|
| High blood sugar | over 16 mmol/L or 300 mg/dL (though with low insulin, lower as well...) |
| Dehydration | (skin doesn't jump back after pulling a bit gums are tacky or dry)[2] |
| Not eating for over 12 hours | due to Inappetance or Fasting |
| Vomiting | |
| Lethargy | |
| Infection or illness | |
| High stress levels | |
| Breath smells like acetone (nail-polish remover) or fruit. | |
Note that the triggers and signs are somewhat interchangeable because ketoacidosis is, once begun, a set of vicious circles which will make itself worse. So dehydration, hyperglycemia, fasting, and presence of ketones are not only signs, they're also sometimes triggers.
|
In a diabetic, any urinary ketones above trace, or any increase in urinary ketone level, or trace urinary ketones plus some of the symptoms above, are cause to call an emergency vet immediately, at any hour of the day. | ||
When to come to the vet
Trace urinary ketones may or may not be an emergency, depending on the case. If a vet is unavailable, look for some of the other signs or triggers, and try to remedy any you can. Give extra water and food, by syringe if necessary. If it's nearly time for an insulin shot, give one. Continue testing and call a vet when possible.
DKA cannot be treated at home. Veterinary care for DKA involves intravenous (IV) fluids to flush the animal's system of the ketones and when necessary, to replace depleted electrolytes[3][4][5], such as bicarbonate; intravenous or intramuscular fast-acting insulin to bring the blood glucose levels down[6][7]; measured amounts of glucose or force feeding, sometimes by feeding tube, to force the metabolism back from fat-burning to glucose-burning.
Dehydration becomes involved with ketoacidosis, which can mean that subcutaneous insulin injections are not properly absorbed; when this occurs, intravenous treatment with soluble, short-acting insulin is needed[8],along with rehydrating intravenous fluids.
Veterinary care for DKA may involve a hospital stay of five days or more and cost, in the U.S., $2,000 or more. Some animals are DKA prone, and may have multiple episodes of the condition.
Veterinarians have sometimes been known to send pets home from a DKA episode while still displaying ketones in the urine -- this is often a fatal mistake. Your chances of fixing the problem yourself are slim. If your cat or dog comes back from the hospital and still has ketones showing on urine testing stix, it's usually best to go right back to the vet's. Or to a better vet's.
How it happens
When there's not enough insulin to allow conversion of glucose to energy, the body begins to break down fat cells, which produce fatty acids. These fatty acids are converted to ketones which can fuel the brain in emergencies.
Our bodies normally are "fueled" by burning glucose; they are able to do this provided they have enough insulin (normally or by injection). When there's not enough insulin to allow the body to burn glucose for energy, it begins metabolizing fat to fuel its cells. In particular, the brain cannot go without energy even for a second, so it demands fat conversion to ketones when glucose energy is unavailable[9]. Continuing this process using fat and ketones instead of glucose without sufficient insulin intervention is the path to ketoacidosis.
Adapted from the Wikipedia:
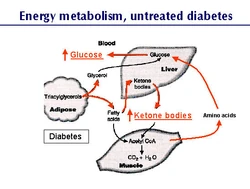
Energy Production-Untreated/Inadequately Treated Diabetes-without enough insulin to regulate fat & carbohydrate metabolism, the process intensifies. The liver, despite high blood glucose levels, produces still more in gluconeogenesis. It also speeds up the transformation of fatty acids resulting in ketones.
Normally, ketone bodies are produced in minuscule quantities, feeding only part of the energy needs of the heart and brain. When insulin is inadequate, fat must be turned into ketones for energy instead, and they rapidly become a major component of the brain's fuel. As a result, the bloodstream is filled with an increasing amount of glucose that it cannot use (as the body continues adding glucose to the blood with gluconeogenesis and perhaps also glycogenolysis). This extra glucose significantly increases its osmolality.
At the same time, massive amounts of ketone bodies are produced, which in addition to increasing the osmolal load of the blood, are acidic. As a result, the pH of the blood begins to change. The trace element balance of the system is altered by falling bicarbonate blood levels and rising serum potassium levels. The potassium level of the body as a whole is reduced by the polyuria of ketoacidosis[10][11]. There can be changes in breathing (deep, sighing breaths) because the ketones themselves are acids. Any type of acidosis can affect the respiratory system.
Glucose begins to spill into the urine as the proteins responsible for reclaiming it from urine reach maximum capacity. As it does so, it takes a great deal of body water with it, resulting in dehydration[12]. Dehydration worsens the increased osmolality of the blood, and forces water out of cells and into the bloodstream in order to keep vital organs perfused. The vicious cycle is now set, and if untreated will lead to coma and death.
How likely is it?
Since diabetic dogs are considered insulin-dependent--unable to naturally provide any of their own insulin needs once diagnosed with diabetes--they are prone to ketoacidosis[13]. About 40% of newly-diagnosed canine diabetics have some amount of ketones when they are brought to the vet[14].
Undiagnosed diabetic cats are also likely to be ketoacidotic by the time they're brought to a vet, but not all cats are prone to ketoacidosis. It is suggested that cats who are prone to ketoacidosis may benefit from a slightly lowered protein diet, [15], but note that this is lowered from an ideal mouse diet, not from an average domestic cat-food diet! Note also that some ketone-prone cats are ketone-prone due to pancreatitis, which requires just the opposite, a lowered-fat diet. Best to stick with an ideal cat diet[16][17] unless you know for certain otherwise.
Testing for ketones
The usual method of testing for ketones is with urine testing stix, available at any pharmacy.
At present there is only one device for consumers who wish to test blood instead of urine for ketones--Abbott's Precision Xtra[18] glucometer. The meter is known by the brand name Precision/Optimum/Xceed outside of the US[19].
The premise behind blood testing for ketones is the same as that for favoring glucose testing of blood over urine[20][21]. The urine ketone measurement, like urine glucose measurement, can be hours old; testing blood for both gives current values as of testing time[22][23][24][25].
Children with Diabetes[26] advises every family with a child with diabetes should have this type of meter because of its blood ketone testing ability. The ketone test strips are about $30 for 10 individually-wrapped strips. The Precision Xtra also does blood glucose testing with standard blood glucose test strips made for use with the meter.
Further Reading
- Wiki cases--Feline DKA
- Felinediabetes.com on Ketoacidosis
- The "hows and whys of ketones" from an FDMB posting
- A quick summary of DKA in cats
- Dr. Elizabeth Hodgkins: Ketones and Low-Carb diet
- Diabetic crisis in Cats & Concurrent Disease-North American Veterinary Conference-2005
- A chapter about ketone testing from the tenth edition of Understanding Diabetes by H. Peter Chase, MD, a book about living with insulin-dependent diabetic humans
- Wikipedia:Diabetic Ketoacidosis
- Treating the Complicated Diabetic Patient--Dr. David Church--WSAVA 2001
- Understanding Diabetic Ketoacidosis--WSAVA 2005
- Emergency veterinary hospitals worldwide
- Metabolic Changes in Diabetic Ketoacidosis--The Genetic Landscape of Diabetes
References
- ↑ Blood Ketone Testing Meter--Abbott's Precision Xtra
- ↑ Pet Education.com-Drs. Foster & Smith-Water: A Nutritional Requirement
- ↑ Pet Education.com-Drs. Foster & Smith-Potassium Requirements & Deficiencies
- ↑ Pet Education.com-Drs. Foster & Smith-Sodium & Chloride Requirements & Deficiencies
- ↑ RxEd.org-Hypokalemia-Low Blood Potassium
- ↑ Critical Care Monitoring Considerations for the Diabetic Patient-Clinical Techniques in Small Animal Practice-2002
- ↑ Low-dose Intramuscular Insulin Therapy for Diabetic Ketoacidosis in Dogs-Journal of the American Veterinary Medical Association-1981
- ↑ American College of Emergency Physicians-Pediatric Endocrine Emergency Answer Sheet
- ↑ Energy Metabolism Explained
- ↑ Ketoacidosis
- ↑ Providing Care for Diabetic Veterinary Patients-IJPC-2000-Page 2
- ↑ Washington State University: Fluid Therapy in Diabetes Mellitus
- ↑ Better Medicine-E-Newsletter-June 2006
- ↑ Beyond Insulin Therapy: Achieving Optimal Control in Diabetic Dogs Drs. Fleeman & Rand-U-Queensland--2005
- ↑ BD Diabetes-Diet & Exercise for the Diabetic Cat
- ↑ Dr. Lisa Pierson's Cat Diet Page
- ↑ Maxshouse Feline Nutrition reference page
- ↑ Abbott's Precision Xtra
- ↑ Abbott's Precision/Optimum/Xceed
- ↑ Point of Care Test Identifies Diabetic Ketoacidosis at Triage-Academic Emergency Medicine-June 2006
- ↑ Exploring the Clinical Utility of Blood Ketone Levels in ER Department Assessment of Pediatric Patients-Emergency Medicine Journal-October 2006
- ↑ Value of Testing Blood for Ketones Over Testing Urine
- ↑ Evaluation of an Electrochemical Sensor for Measuring Blood Ketones-Diabetes Care 2000
- ↑ Accuracy of an Electrochemical Sensor for Measuring Capillary Blood Ketones by Fingerstick Samples During Metabolic Deterioration After Continuous Subcutaneous Insulin Infusion Interruption in Type 1 Diabetic Patient--Diabetes Care 2003
- ↑ Accuracy of Serum β-Hydroxybutyrate Measurements for the Diagnosis of Diabetic Ketoacidosis in 116 Dogs-Journal of Veterinary Internal Medicine 2002
- ↑ Meter Which Tests Blood for Ketones